Hey there, dear reader! Thanks for dropping by my blog. Today, I want to share something that I think many of us can relate to – the dreaded infected wisdom tooth.
I've personally experienced this, and I know how painful and worrisome it can be.
But don't worry, I've got your back! I've done my homework and put together this comprehensive guide on infected wisdom tooth. We'll cover everything from causes and symptoms to treatment options and prevention strategies. So, let's dive in and explore the world of infected wisdom teeth together.
Infected Wisdom Tooth: What's the Deal?
Wisdom tooth, also known as third molars, are the last teeth to develop and erupt in our mouths.
They typically appear between the ages of 17 and 25. However, not everyone has enough space in their mouth to accommodate these late bloomers, which can lead to a variety of dental issues, including infection.
An infected wisdom tooth, also known as pericoronitis, occurs when bacteria accumulate around the partially erupted or impacted wisdom tooth, leading to inflammation and infection in the surrounding gum tissue.
It's a common issue among young adults, and it's definitely something you should be aware of.
Discover My Ultimate Checklist for Maintaining Healthy Teeth and Gums on a Daily and Weekly Basis
From Brushing to Flossing: Follow My 7-Step Checklist to Achieve Optimal Dental Health and Prevent Oral Problems.
What Causes Infected Wisdom Tooth?
There are several factors that can contribute to an infected wisdom tooth. Here are the most common causes:
- Impacted wisdom teeth: When a wisdom tooth doesn't fully erupt or remains trapped beneath the gum line, it's considered impacted. This makes it difficult to clean and creates a perfect breeding ground for bacteria.
- Partially erupted wisdom teeth: Sometimes, a wisdom tooth may partially erupt, leaving a flap of gum tissue covering part of the tooth. This flap, called an operculum, can trap food particles and bacteria, leading to infection.
- Poor oral hygiene: Neglecting your oral care routine, such as not brushing and flossing regularly, can lead to a buildup of bacteria and plaque around your wisdom teeth, increasing the risk of infection.
- Crowding: When there isn't enough room in your mouth for your wisdom teeth to fully erupt, they can become crowded and difficult to clean, making them more susceptible to infection.
Recognizing the Symptoms: How to Know If Your Wisdom Tooth Is Infected
Knowing the symptoms of an infected wisdom tooth can help you identify the problem and seek treatment promptly. Here's what you should watch out for:
- Pain and swelling: One of the most common symptoms of an infected wisdom tooth is pain and swelling in the affected area. The pain can be throbbing or sharp and may worsen when biting or chewing.
- Redness and inflammation: The gum tissue around the infected wisdom tooth may appear red, swollen, and inflamed.
- Bad taste or odor: An infected wisdom tooth can cause a foul taste in your mouth or persistent bad breath.
- Difficulty opening your mouth: In some cases, the swelling and pain may make it difficult to open your mouth fully.
- Fever and general malaise: As with any infection, an infected wisdom tooth can cause fever, chills, and a general feeling of being unwell.
If you're experiencing any of these symptoms, it's crucial to visit your dentist as soon as possible for a proper diagnosis and treatment plan.
Treatment Options for Infected Wisdom Tooth

There's no need to panic if you suspect you have an infected wisdom tooth. There are several effective treatment options available to help you get back to feeling your best. Here's what your dentist may recommend:
1. Antibiotics: In some cases, your dentist may prescribe antibiotics to help clear the infection. It's important to follow your dentist's instructions and take the full course of antibiotics, even if you start to feel better before you've finished the medication.
2. Pain relief: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and reduce inflammation. Be sure to follow the recommended dosage instructions and consult your dentist or doctor if you're unsure.

3. Rinsing with warm salt water: Rinsing your mouth with warm salt water several times a day can help soothe the affected area and promote healing. Mix half a teaspoon of salt in a glass of warm water, swish it around your mouth, and then spit it out.

4. Oral hygiene: Maintaining good oral hygiene is essential during the healing process. Continue to brush your teeth gently, taking care around the infected area, and floss daily.

5. Wisdom tooth extraction: In many cases, the best course of action is to remove the infected wisdom tooth. This can be done by a dentist or oral surgeon, depending on the complexity of the extraction. Wisdom tooth extraction is a common procedure, and your dental professional will provide you with detailed aftercare instructions to ensure a smooth recovery.
Maintain good oral hygiene: Brush your teeth twice a day with a soft-bristle toothbrush, floss daily, and use an antibacterial mouthwash to keep your mouth clean and healthy.
Regular dental checkups: Visiting your dentist every six months for a checkup and cleaning can help detect and address any issues with your wisdom teeth before they become problematic.
Eat a balanced diet: A well-balanced, nutrient-rich diet can help support your immune system and overall oral health. Make sure you're getting enough vitamins and minerals, especially vitamin C, which is essential for maintaining healthy gums.
Stay hydrated: Drinking water throughout the day helps wash away bacteria and food particles, reducing the risk of infection.
Consider early extraction: If your dentist determines that your wisdom teeth are likely to cause issues in the future, they may recommend having them extracted before problems arise. This proactive approach can help prevent infections and other complications associated with impacted or partially erupted wisdom teeth.
Simple extraction: If your wisdom tooth has fully erupted and is easily accessible, your dentist may perform a simple extraction. This procedure involves using a tool called an elevator to loosen the tooth, followed by forceps to remove it.
Surgical extraction: If your wisdom tooth is impacted or partially erupted, a surgical extraction may be necessary. This procedure is typically performed by an oral surgeon and involves making a small incision in the gum tissue to expose the tooth, and then removing it in sections if needed.
Local anesthesia: Your dentist will numb the area around the tooth with a local anesthetic, such as lidocaine. You'll be awake during the procedure but won't feel any pain.
Nitrous oxide (laughing gas): Nitrous oxide is a mild sedative that can help you feel more relaxed during the extraction. You'll still be awake and able to communicate with your dentist, but you may feel a bit drowsy.
Oral sedation: Your dentist may prescribe a sedative medication to be taken before the appointment, which can help you feel more relaxed and drowsy during the procedure.
IV sedation: In some cases, your dentist or oral surgeon may recommend intravenous (IV) sedation, which allows you to be in a deeply relaxed state but still conscious during the extraction.
General anesthesia: For complex extractions or patients with high levels of anxiety, general anesthesia may be an option. This involves being completely unconscious during the procedure.
Bite on gauze: Your dentist will place a gauze pad over the extraction site to control bleeding. Bite down gently but firmly for the first hour or as directed by your dentist.
Rest and elevate your head: Take it easy for the first 24 hours and avoid lying flat. Keep your head elevated to minimize swelling and bleeding.
Apply ice packs: Applying ice packs to the outside of your cheek can help reduce swelling. Use the ice for 20 minutes on and 20 minutes off during the first day.
Stick to a soft diet: For the first few days, eat soft foods like yogurt, applesauce, and mashed potatoes. Gradually reintroduce solid foods as your comfort level allows.
Avoid using straws: The suction created by using a straw can dislodge the blood clot that forms in the extraction site, leading to a painful condition called dry socket. Avoid using straws for at least a week after your extraction.
Don't smoke: Smoking can also dislodge the blood clot and delay healing. Refrain from smoking for at least 72 hours after the extraction.
Gentle oral care: Continue to brush your teeth gently, avoiding the extraction site for the first few days. Rinse your mouth with warm salt water after meals to help keep the area clean.
Follow your dentist's instructions: Your dentist may provide specific instructions regarding pain relief, antibiotics, or other medications. Be sure to follow their recommendations and contact them if you have any concerns during your recovery.
Severe or worsening pain: While some pain is expected, if it worsens or doesn't improve with over-the-counter pain relievers, it could indicate a problem such as a dry socket or infection.
Signs of infection: Fever, pus or discharge from the extraction site, and increased swelling or redness could indicate an infection that requires prompt attention.
Uncontrolled bleeding: Some bleeding is normal, but if it doesn't subside after a few hours or becomes heavy, contact your dentist.
Persistent numbness: If you experience numbness in your tongue, lips, or chin for an extended period after the anesthesia has worn off, it could indicate nerve damage. Contact your dentist to discuss your symptoms.
Reduced risk of infection and dental issues: With your problematic wisdom teeth gone, you'll have a lower chance of developing infections, gum disease, and tooth decay in the area.
Easier oral hygiene: Without crowded or impacted wisdom teeth, it'll be simpler to brush and floss effectively, promoting better overall oral health.
No more pain or discomfort: Wisdom teeth can cause pain and pressure as they try to erupt or shift neighboring teeth. By removing them, you can say goodbye to that discomfort.
Preventing damage to adjacent teeth: Impacted wisdom teeth can damage the roots of nearby teeth. Extraction can prevent such damage and help preserve your other teeth.
Prevention Strategies: Keeping Infected Wisdom Teeth at Bay
While it's not always possible to prevent an infected wisdom tooth, there are some steps you can take to minimize your risk:
Wisdom Tooth Extraction: What to Expect?
If your dentist recommends extracting your infected wisdom tooth, it's natural to feel a bit anxious. But don't worry, I'm here to walk you through the process so you know what to expect.
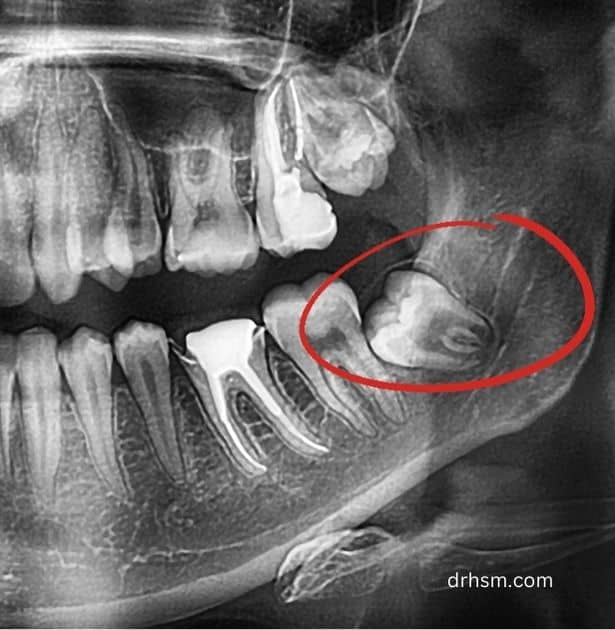
Consultation and X-rays
Before the extraction, your dentist will schedule a consultation to discuss the procedure and any concerns you may have. They will also take X-rays to assess the position of your wisdom teeth and determine the complexity of the extraction.
Types of Extraction
There are two main types of wisdom tooth extraction:
Anesthesia Options
There are several anesthesia options available to ensure your comfort during the extraction:
Your dentist will discuss your anesthesia options and help you choose the best one for your needs and comfort level.
Aftercare and Recovery
Following the extraction, it's essential to follow your dentist's aftercare instructions to ensure a smooth recovery. Here are some general tips for post-extraction care:
When to Call Your Dentist
While some pain, swelling, and discomfort are normal after a wisdom tooth extraction, there are certain situations where you should contact your dentist or oral surgeon. Reach out to them if you experience any of the following:
Long-term Considerations: What to Expect After Your Wisdom Teeth Are Gone
Once you've recovered from your wisdom tooth extraction, you can expect to enjoy some long-term benefits, such as:
Discover My Ultimate Checklist for Maintaining Healthy Teeth and Gums on a Daily and Weekly Basis
From Brushing to Flossing: Follow My 7-Step Checklist to Achieve Optimal Dental Health and Prevent Oral Problems.
Remember, regular dental checkups and good oral hygiene habits are still essential for maintaining a healthy mouth, even after your wisdom teeth have been removed.
And there you have it!
This comprehensive guide on infected wisdom teeth should have you feeling well-informed and ready to tackle any issues that may arise with your wisdom teeth.
Don't hesitate to reach out to your dentist if you have any concerns or questions. Here's to a lifetime of healthy, happy smiles!
